Manual Osteopathy for Myofascial Pain Syndrome
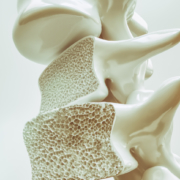
Myofascial pain syndrome (MPS) is a common yet often misunderstood condition characterized by chronic muscle pain and discomfort. While the exact cause of MPS can vary, it often involves the development of trigger points within the muscles and fascia, leading to pain, stiffness, and reduced range of motion. For individuals living with MPS, finding effective relief can be a challenging journey. However, manual osteopathy offers a holistic approach that can help alleviate symptoms and improve overall well-being.
Understanding Myofascial Pain Syndrome
Before delving into the benefits of manual osteopathy for MPS, it’s essential to understand the nature of this condition. Myofascial pain syndrome involves the development of trigger points—hyperirritable spots within the muscle tissue—that can cause referred pain, muscle stiffness, and a range of other symptoms. These trigger points often develop due to muscle overuse, injury, poor posture, or stress, leading to tension and discomfort in affected areas.The
Role of Manual Osteopathy
Manual osteopathy is a hands-on therapy that focuses on restoring balance and function to the body’s musculoskeletal system. Unlike conventional medicine, which often treats symptoms in isolation, manual osteopathy takes a holistic approach, addressing the underlying causes of pain and dysfunction. By manipulating the muscles, joints, and connective tissues, manual osteopaths can help release tension, improve circulation, and restore proper alignment, facilitating the body’s natural healing process.
Benefits of Manual Osteopathy for MPS
Targeted Pain Relief:
Manual osteopathy techniques, such as soft tissue manipulation and myofascial release, target the trigger points and tight muscles associated with MPS. By applying gentle pressure and stretching techniques, manual osteopaths can help release tension, reduce pain, and improve muscle function.
Improved Range of Motion:
Individuals with MPS often experience stiffness and restricted movement in affected muscles and joints. Manual osteopathy techniques, such as joint mobilization and stretching exercises, can help improve flexibility and range of motion, allowing for greater mobility and ease of movement.
Stress Reduction:
Chronic pain conditions like MPS can take a toll on mental and emotional well-being, leading to increased stress and anxiety. Manual osteopathy treatments not only address physical symptoms but also promote relaxation and stress reduction. By releasing tension in the muscles and promoting relaxation responses in the body, manual osteopathy can help alleviate stress and improve overall mental health.
Enhanced Circulation:
Poor circulation can exacerbate symptoms of MPS by depriving muscles of oxygen and nutrients needed for healing. Manual osteopathy techniques, such as massage and gentle manipulation, can help improve blood flow to affected areas, promoting healing and reducing inflammation.
Individualized Treatment Plans:
One of the key benefits of manual osteopathy is its personalized approach to care. Manual osteopaths assess each patient’s unique needs and develop customized treatment plans tailored to their specific condition and goals. By addressing the root causes of MPS and considering factors such as lifestyle, posture, and biomechanics, manual osteopaths can provide comprehensive care that addresses the whole person.Non-Invasive and
Drug-Free:
Unlike some conventional treatments for MPS, such as medications or injections, manual osteopathy is non-invasive and drug-free. This makes it a safe and natural option for individuals seeking relief from chronic pain without the risk of side effects or dependency.
Myofascial pain syndrome can be a debilitating condition that affects every aspect of daily life. However, with the right approach to treatment, individuals with MPS can find relief and regain control over their health and well-being.
Manual osteopathy offers a holistic approach that addresses the underlying causes of MPS, providing targeted pain relief, improved mobility, and enhanced overall wellness. By working with a skilled and compassionate manual osteopath, individuals with MPS can embark on a journey towards a pain-free and vibrant life.
To book an appointment, give us a call @ 780-455-2112 to get started. To learn more click here.